Dr Iqbal Poetry in Hindi
If the "Health Freedom" movement has its way, everyone in the United States will be able to practice medicine. It may be quack medicine but that doesn't seem to bother them. Short of that, chiropractors, naturopaths and acupuncturists are aiming to reinvent themselves primary care providers and even physicians. As David Gorski pointed out, this will reduce medical doctors to just another iteration of physician, the "allopathic" type, equal in stature to the chiropractic, naturopathic and acupuncture types. These "physicians" already call themselves "doctor" (e.g., "Doctor of Oriental Medicine") and claim to graduate from four-year "doctoral" programs. This despite the fact that their schools operate outside the mainstream American university system and avoid some of the basics of typical graduate programs, such as entrance exams, as well as the extensive clinical training required for medical doctors.
Consumers are confused by all of this, and who wouldn't be? In 2008 and 2010, surveys done for the American Medical Association by outside firms revealed that many patients did not know the qualifications of their healthcare provider. The comparisons were between allied health professions (e.g., audiologists and nurse practitioners) and medical doctors, but chiropractors were included. In 2008, 38 per cent of those surveyed (n=850) thought chiropractors were medical doctors, although that dropped to 31 per cent in 2010. Still, we are talking about roughly one-third of the survey participants.
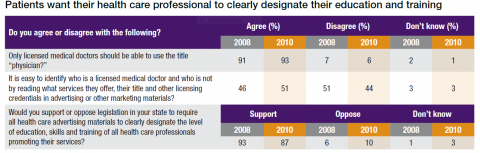
The surveys also asked about the use of the term "physician" and confusion in advertising materials.
(Sorry, my visual aids are not as titillating as Dr. Gorski's, but I couldn't find any Penthouse covers relevant to this topic.)
Etiquette weighs in: a digression
Before we go any further, let's digress into a topic raised in the comments of a previous post: who should use the title "Doctor," at least in what is referred to somewhat quaintly as "social settings." But first, a disclaimer: This advice only applies to the United States. Your country may have a totally different set of rules.
I consulted the experts on this, that is, the etiquette experts, people no one pays much attention to anymore. I found what is known in the legal field as a "split of authority." Miss Manners (Judith Martin) says "Dr." should be reserved for those in the medical profession, although she also thinks people should be called what they want to be called. So, if someone insists, then "Dr." it is. On the other hand, Letitia Baldridge, who served as social secretary to Jacqueline Kennedy Onassis when she was first lady, is (or was, she passed away last year) of the opinion that your academic title is also your social setting title. Emily Post sides with Miss Manners. In social settings, she advises one start with by addressing both Ph.Ds and medical doctors as "Dr." and if the former prefer some other title, they will tell you.
So now you know.
Truth in Healthcare Marketing
A bill introduced in the U.S. House of Representatives, with bipartisan support, aims to clear things up in the professional, if not social, setting. H.R. 1427, the "Truth in Healthcare Marketing Act," would prohibit any "deceptive or misleading" statement or act that "misrepresents" a person's "education, training, degree, license or clinical expertise." If H.R. 1427 becomes law, such misrepresentations would be a violation of the Federal Trade Commission Act, which prohibits, among other things, any unfair or deceptive advertising or marketing practice.
Under the proposed Act, the information must be deceptive or misleading, but the bill also specifies that it must "misrepresent" the education, training, degree, license or clinical expertise. But if information is deceptive or misleading, I would argue that it by definition it "misrepresents" so I am not clear whether, as a practical matter, that is an additional requirement or not.
In any event, misrepresentation of a license or degree should be pretty clear cut, but I'm not sure where the boundaries might fall around misrepresentation of one's education, training, or clinical expertise. Of course, there are always the egregious cases, like the Colorado chiropractor claiming to be an endocrinologist whose treatments could "reverse diabetes." Having a wimpy chiropractic board administer a delicate wrist slap is one thing; having the Feds after you is quite another.
As we've noted on SBM, both naturopaths and chiropractors claim their education and training is sufficient to practice as a primary care physician. They promote the idea that their schools offer an education that is either the equivalent of, or close to, that of a medical doctor. A chart handed out by naturopaths in support of their Colorado licensing bill claims they have more hours of education in pharmacology than medical doctors. And a chart published by the American Chiropractic Association (ACA), posted below, purports to show that chiropractic students have more combined classroom and clinical hours than medical students. (The ACA made similar overblown statements in a brief filed with a Colorado court.) Assuming these claims are made in a context otherwise covered by the Act (such as advertising by a chiropractor) would representations like this pass muster under the proposed "Truth in Healthcare Marketing Act of 2013"?
Let's look at a description of chiropractic education from the American Chiropractic Association's website. [Emphasis added.]
Chiropractic Education
Educational requirements for doctors of chiropractic are among the most stringent of any of the health care professions.
The typical applicant at a chiropractic college has already acquired nearly four years of pre-medical undergraduate college education, including courses in biology, inorganic and organic chemistry, physics, psychology and related lab work. Once accepted into an accredited chiropractic college, the requirements become even more demanding — four to five academic years of professional study are the standard. Because of the hands-on nature of chiropractic, and the intricate adjusting techniques, a significant portion of time is spent in clinical training.
Doctors of chiropractic — who are licensed to practice in all 50 states, the District of Columbia, and in many nations around the world — undergo a rigorous education in the healing sciences, similar to that of medical doctors. In some areas, such as anatomy, physiology, and rehabilitation, they receive more intensive education than most medical doctors or physical therapists.

Like other primary health care doctors, chiropractic students spend a significant portion of their curriculum studying clinical subjects related to evaluating and caring for patients. Typically, as part of their professional training, they must complete a minimum of a one-year clinical-based program dealing with actual patient care. In total, the curriculum includes a minimum of 4,200 hours of classroom, laboratory and clinical experience. [Then why does the chart say 4820?] The course of study is approved by an accrediting agency which is fully recognized by the U.S. Department of Education. This has been the case for more than 25 years.
Before they are allowed to practice, doctors of chiropractic must pass national board examinations and become state-licensed. Chiropractic colleges also offer post-graduate continuing education programs in specialty fields ranging from sports injuries and occupational health to orthopedics and neurology. These programs allow chiropractors to specialize in a healthcare discipline or meet state re-licensure requirements.
This extensive education prepares doctors of chiropractic to diagnose health care problems, treat the problems when they are within their scope of practice and refer patients to other health care practitioners when appropriate.
[Hmmm. The ACA says that "intricate adjusting techniques" are taught in chiropractic college as part of the "significant portion of time" spent in clinical training? And what do chiropractors "adjust"? Subluxations! So much for the claims that detecting and correcting subluxations is not emphasized and is taught only as a historical concept in chiropractic schools.]
Misleading or deceptive?
Before we parse this description, note some of the relevant criteria by which the information is judged under the FTC Act.
- No intent to deceive must be present. Innocent misrepresentations are covered by the FTC Act.
- How an average or unsophisticated person, not the expert, would view the information is the standard. Would it mislead an average consumer?
- The information is looked at as a whole and can be deemed deceptive even though the individual statements made are literally true.
- The claims made must be material to the consumer, that is, the information must be important to consumers and likely to affect their choice of, or conduct regarding, a product or service.
It is interesting to note that the ACA's discussion of chiropractic education may be, for the most part, literally true. (Although I seriously doubt that the chiropractic student's education in anatomy or physiology is more "intensive" than that of a medical student, especially considering their narrow focus on the musculoskeletal system.) But, as we know, literal truth is not the standard. We have to look at the information taken as a whole.
Here is where I think the information might be deceptive or misleading as interpreted by the average consumer who would consider a health care provider's education to be important but who is not familiar with the health professional educational system. Those more familiar with medical education can likely add to my observations.
- Hours and calendar years are used to compare education, when in fact the number of hours or years is not an indication of quality or rigor. (By this standard, elementary school is more demanding than college.) Nor are classroom and clinical hours inclusive of all time spent in learning. What about time spent in independent research?
- While the chart notes the years spent in residency are not included, failing to count those leaves out a substantial and important difference between chiropractic and medical education.
- There is no mention of the chiropractic student's focus on the musculoskeletal system or the fact that medical students have far more education in any number of subjects, such as pharmacology, primary care, and pediatrics as well as the body's other systems, such as cardiovascular and reproductive. Nor do chiropractic students have clinical training in a variety of specialties.
- There is no mention of the focus on the musculoskeletal system in actual chiropractic practice. In fact, chiropractors are referred to as primary health care practitioners.
- The mention of "post-graduate" educational programs leading to "specialties," fails to note that these are mostly limited to courses taken over a number of weekends with little (perhaps no) actual clinical training.
My conclusion is that this description viewed as a whole would leave the average consumer with the false impression that chiropractic education is equal in rigor and breadth to a medical education and qualifies graduates to practice as primary care physicians. Under federal law, this need not be the only interpretation possible to violate the FTC Act, but it is certainly one a reasonable consumer could reach. Again, about one third of survey participants actually thought chiropractors are medical doctors. To the extent that chiropractors use similar information in their advertising and other communications with the public they would be vulnerable to suits claiming violation of the FTC Act.
But that's not all.
The bill also requires the FTC to undertake a study of healthcare professionals to:
- Identify acts and practices constituting a violation of the new law, their frequency, and instances of harm or injury caused.
- Determine whether health care professionals are complying with state laws requiring disclosure of the type of license they hold.
- "Identify instances where any State public policy has permitted acts and practices which violate section 3(a)," the section prohibiting deceptive or misleading statements, discussed above.
I, for one, will be more than happy to "identify . . . State policy" permitting these deceptive practices. For instance:
- Licensing chiropractors, naturopaths and acupuncturists as primary care providers, either explicitly or de facto through wide scopes of practice.
- Effectively giving out licenses to practice quackery by permitting such practices as the "detection" and "correction" of subluxations, prescribing homeopathic "remedies," iridology, cranial sacral therapy, energy healing . . . well, I could go on and on. I will quote state laws and regulations, chapter and verse.
- Allowing self-regulation (including the right to write their own regulations) through the creation of state board dominated by "CAM" practitioners. Once these practitioners are governed by their own boards, which have exclusive jurisdiction to discipline them, it is difficult to hold them accountable.
- Blindly accepting, lock, stock and barrel, whatever education, testing, certification, training, continuing education, and the like these practitioners chose to create for themselves without any outside scrutiny (other than the Department of Education accrediting agency requirements, which reject science as an appropriate standard for health care education).
If done properly, this report could be at least a PR disaster for CAM providers. (Or not. Government reports about problems with dietary supplements do not seem to have tempered the public's enthusiasm for supplements.) And it might even embarrass some states into actually instituting reforms, such as, say, a single, science-based standard for all health care practitioners.
If H.R. 1427 becomes law, I'll be sitting by the computer, Federal Trade Commission, waiting for your e-mail. You can reach me through the SBM website.
-
Jann J. Bellamy is a Florida attorney and lives in Tallahassee. She is one of the founders and Board members of the Society for Science-Based Medicine (SfSBM) dedicated to providing accurate information about CAM and advocating for state and federal laws that incorporate a science-based standard for all health care practitioners. She tracks state and federal bills that would allow pseudoscience in health care for the SfSBM website. Her posts are archived here.
View all posts
Source: https://sciencebasedmedicine.org/dr-who/